Cannabis enthält über 100 Cannabinoide und über 300 weitere chemische Verbindungen, die Auswirkungen auf verschiedene Systeme des Körpers haben. Diese beeinflussen Gesundheit und Krankheitszustände. Die chemischen Bestandteile von Cannabis beeinflussen nicht nur das Endocannabinoid-System, sondern eine Vielzahl an Einheiten in unserem Körper.
Phytocannabinoide
Die Forschung zeigt, dass die Wirkung von Phytocannabinoiden durch Duftstoffe, die von der Cannabispflanze produziert werden, sogenannten Terpenen, beeinflusst werden könnte. Diese Wechselwirkung würde zum Entourage-Effekt führen. Dieser Ansatz besagt, dass Cannabinoide besser wirken, wenn sie in Verbindung mit einer Reihe anderer Cannabinoide, Terpene, Flavonoide und Verbindungen, die in Cannabis enthalten sind, eingenommen werden, als wenn sie als isolierte Wirkstoffe vorliegen.
Tetrahydrocannabinol (THC)
THC ist ein berauschendes und psychoaktives Cannabinoid. Es kommt in zwei Formen vor: Delta-9-THC und Delta-8-THC. Delta-9-THC ist das bekannteste Cannabinoid der Cannabispflanze und wird normalerweise umgangssprachlich als THC bezeichnet. Es kann vielfältige sensorische und geistige Wirkungen hervorrufen, wie z. B. leichte Träumerei, ein Gefühl der Ausgeglichenheit, eine gesteigerte Sensibilität, aber auch therapeutische Wirkungen.
THC ist zwar nicht allein für die psychoaktive Wirkung von Cannabis verantwortlich, aber es ist der wichtigste psychoaktive Bestandteil. THC wird nur aktiviert, wenn es einen Hitzeprozess durchläuft. Dabei wird es von seiner ursprünglichen chemischen Struktur THCA (Säureform) zu THC. THC bindet und aktiviert die CB1-Rezeptoren, die hauptsächlich im zentralen Nervensystem vorzufinden sind, was zu dem bekannten “High“ und anderen psychischen Wirkungen führt.
Cannabidiol (CBD)
Cannabidiol (CBD) ist heutzutage ein bekanntes Cannabinoid und steht im Mittelpunkt vieler medizinischer Forschungsarbeiten. CBD gilt als "nicht psychoaktiv", verändert allerdings in gewissem Maße das Bewusstsein, wie durch seine Wirksamkeit bei Angstzuständen nachgewiesen wird. Cannabidiol ist nach THC das am zweithäufigsten vorkommende Cannabinoid in der Hanfpflanze. CBD entsteht durch die Erhitzung bzw. Decarboxylierung von Cannabidiol-Säure (CBDA). Die meisten Cannabissorten haben niedrigere CBD-Konzentrationen als THC. CBD hat viele potenzielle therapeutische Vorteile, die durch Verbraucher immer wieder bestätigt werden.
Die Auswirkungen von CBD auf das Gehirn und den Körper sind ziemlich kompliziert. Es ist höchstwahrscheinlich, dass die wohltuenden Wirkungen des CBD über verschiedenste biologische Wege ablaufen und nicht nur über einen einzigen Vorgang. Es bedarf weiterer Forschung, um die Mechanismen vollständig zu verstehen, durch die CBD Beschwerden wie zum Beispiel Krampfanfälle lindert.
Im Gegensatz zu vielen pharmazeutischen Wirkstoffen mit nur einem Wirkungsmechanismus ist CBD eine medizinische Wunderwaffe mit einem überzeugenden Nebenwirkungsprofil und großem Therapiepotenzial.
Terpene
Terpene sind die Hauptbestandteile der ätherischen Öle, die in verschiedenen Cannabissorten enthalten sind. Diese Substanzen sind für die charakteristischen Geruchs- und Geschmacksnoten verantwortlich. Terpene werden von verschiedenen Pflanzen produziert, insbesondere von Nadelbäumen. Viele der Terpene stehen im Zusammenhang mit den Schutzmechanismen der Pflanze gegen Pflanzenschädlinge und die Umwelt.
Das Wort Terpen findet seinen Ursprung in Terpentin, welches der Saft von abgeholzten Bäumen ist oder auch aus Holz destilliert wird.
Terpentin wurde in der alten chinesischen Medizin gegen Zahnschmerzen und Atembeschwerden eingesetzt. Terpene sind sehr flüchtig und “verdampfen“ bei mäßigen Temperaturen schnell. Aus diesem Grund riecht die Luft morgens frischer, da Pflanzen dann ihre maximale Konzentration an Terpenen freisetzen, bevor sie im Laufe des Tages von der Sonne verdunstet werden.
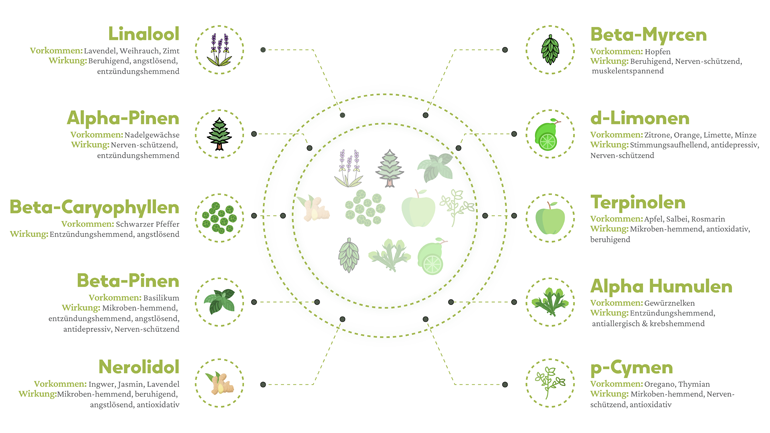
Die wichtigsten Terpene in Cannabis sind A-Pinen (auch in Kiefernnadeln und Rosmarin enthalten), Linalool (auch in Lavendel und Weihrauch enthalten), Beta-Caryophyllen (auch in schwarzem Pfeffer enthalten), Myrcen (auch in Hopfen enthalten) und Limonen, das nach Zitronen riecht und in Zitrusfrüchten enthalten ist.
Wie die Cannabinoide haben auch die Terpene Eigenschaften, die den medizinischen Wert einer Pflanze unterstreichen.
Terpene verleihen Früchten, Blumen, Gemüse und Gewürzen ihren angenehmen Geruch. Ferner haben diese Stoffe auch krebshemmende, entzündungshemmende, angstlösende, schlaffördernde und stimmungsaufhellende therapeutische Eigenschaften.